Acquired Flat Foot Surgery
Overview
Dysfunction of the tibialis posterior tendon is a common condition and a common cause of acquired flatfoot deformity in adults. Women older than 40 are most at risk. Patients present with pain and swelling of the medial hindfoot. Patients may also report a change in the shape of the foot or flattening of the foot. The foot develops a valgus heel (the heel rotates laterally when observed from behind), a flattened longitudinal arch, and an abducted forefoot. Conservative treatment includes non-steroidal anti-inflammatory drugs, rest, and immobilisation for acute inflammation; and orthoses to control the more chronic symptoms. Surgical treatment in the early stages is hindfoot osteotomy combined with tendon transfer. Arthrodesis of the hindfoot, and occasionally the ankle, is required in the surgical treatment of the later stages of tibialis posterior dysfunction. 
Causes
There are a number of theories as to why the tendon becomes inflamed and stops working. It may be related to the poor blood supply within the tendon. Increasing age, inflammatory arthritis, diabetes and obesity have been found to be causes.
Symptoms
Symptoms are minor and may go unnoticed, Pain dominates, rather than deformity. Minor swelling may be visible along the course of the tendon. Pain and swelling along the course of the tendon. Visible decrease in arch height. Aduction of the forefoot on rearfoot. Subluxed tali and navicular joints. Deformation at this point is still flexible. Considerable deformity and weakness. Significant pain. Arthritic changes in the tarsal joints. Deformation at this point is rigid.
Diagnosis
Clinicians need to recognize the early stage of this syndrome which includes pain, swelling, tendonitis and disability. The musculoskeletal portion of the clinical exam can help determine the stage of the disease. It is important to palpate the posterior tibial tendon and test its muscle strength. This is tested by asking patient to plantarflex and invert the foot. Joint range of motion is should be assessed as well. Stiffness of the joints may indicate longstanding disease causing a rigid deformity. A weightbearing examination should be performed as well. A complete absence of the medial longitudinal arch is often seen. In later stages the head of the talus bone projects outward to the point of a large "lump" in the arch. Observing the patient's feet from behind shows a significant valgus rotation of the heel. From behind, the "too many toes" sign may be seen as well. This is when there is abducution of the forefoot in the transverse plane allowing the toes to be seen from behind. Dysfunction of the posterior tibial tendon can be assessed by asking the patient to stand on his/her toes on the affected foot. If they are unable to, this indicates the disease is in a more advanced stage with the tendon possibly completely ruptured.
Non surgical Treatment
Nonoperative treatment of stage 1 and 2 acquired adult flatfoot deformity can be successful. General components of the treatment include the use of comfort shoes. Activity modification to avoid exacerbating activities. Weight loss if indicated. Specific components of treatment that over time can lead to marked improvement in symptoms include a high repetition, low resistance strengthening program. Appropriate bracing or a medial longitudinal arch support. If the posterior tibial tendon is intact, a series of exercises aimed at strengthening the elongated and dysfunctional tendon complex can be successful. In stage 2 deformities, this is combined with an ankle brace for a period of 2-3 months until the symptoms resolve. At this point, the patient is transitioned to an orthotic insert which may help to support the arch. In patients with stage 1 deformity it may be possible to use an arch support immediately. 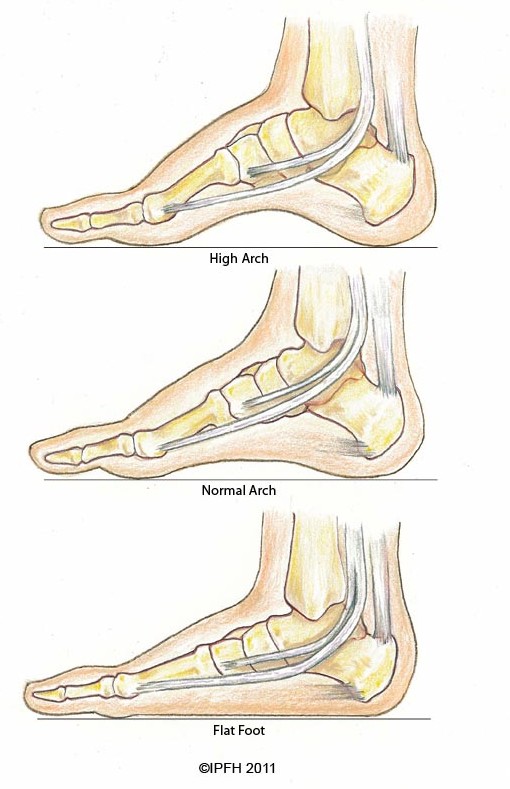
Surgical Treatment
In cases where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The goal of surgery and non-surgical treatment is to eliminate pain, stop progression of the deformity and improve mobility of the patient. Opinions vary as to the best surgical treatment for adult acquired flatfoot. Procedures commonly used to correct the condition include tendon debridement, tendon transfers, osteotomies (cutting and repositioning of bone) and joint fusions. (See surgical correction of adult acquired flatfoot). Patients with adult acquired flatfoot are advised to discuss thoroughly the benefits vs. risks of all surgical options. Most procedures have long-term recovery mandating that the correct procedure be utilized to give the best long-term benefit. Most flatfoot surgical procedures require six to twelve weeks of cast immobilization. Joint fusion procedures require eight weeks of non-weightbearing on the operated foot - meaning you will be on crutches for two months. The bottom line is, Make sure all of your non-surgical options have been covered before considering surgery. Your primary goals with any treatment are to eliminate pain and improve mobility. In many cases, with the properly designed foot orthosis or ankle brace, these goals can be achieved without surgical intervention.